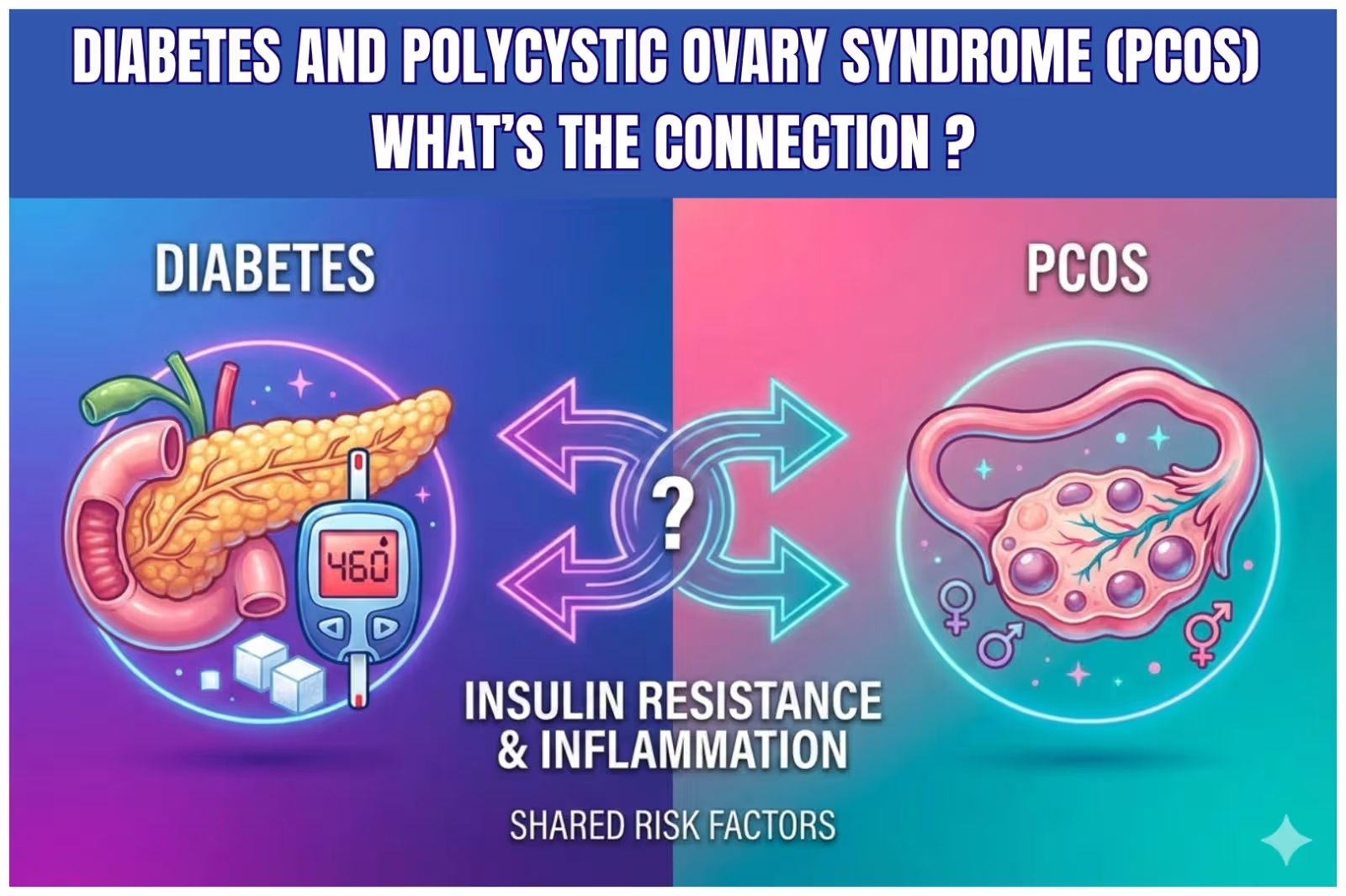
Diabetes and Polycystic Ovary Syndrome (PCOS): What’s the Connection?
Polycystic Ovary Syndrome (PCOS) is one of the most common hormonal disorders affecting women of reproductive age. At the same time, diabetes—especially Type 2 diabetes—is rising rapidly among young women across the world.
What many women don’t realize is that PCOS and diabetes are not separate conditions. They are deeply interconnected, primarily through insulin resistance, hormonal imbalance, and metabolic dysfunction.
If you or someone you know is struggling with irregular periods, weight gain, acne, excess facial hair, mood swings, or difficulty conceiving, understanding this connection can be truly life-changing.
Let’s take a deeper, science-backed and holistic look at how PCOS and diabetes are linked, and how they can be managed naturally and effectively.
What Is PCOS?
Polycystic Ovary Syndrome (PCOS) is a complex endocrine (hormonal) disorder in which the ovaries produce excess androgens (male hormones). This hormonal imbalance disrupts ovulation and menstrual cycles and affects multiple systems of the body.
PCOS is not just a reproductive disorder—it is also a metabolic condition that affects insulin sensitivity, weight, inflammation, and long-term health.
Common Symptoms of PCOS
PCOS symptoms can vary from woman to woman, but the most common include:
Irregular, delayed, or missed periods
Difficulty ovulating or conceiving
Weight gain or difficulty losing weight
Acne and oily skin
Excess facial or body hair (hirsutism)
Hair thinning or hair fall
Dark patches on skin (acanthosis nigricans)
Mood swings, anxiety, or depression
Fatigue and sugar cravings
Because PCOS affects hormones, metabolism, and insulin function, it significantly increases the risk of diabetes and other metabolic disorders.
Read More –PCOS vs PCOD: Simple Guide to Causes, Symptoms, Diagnosis & Treatment
What Is Diabetes?
Diabetes is a chronic metabolic condition in which the body either does not produce enough insulin or cannot use insulin effectively. This results in elevated blood glucose (sugar) levels, which can damage organs over time.
Types of Diabetes Commonly Linked to PCOS
Women with PCOS are at higher risk of developing:
Type 2 Diabetes (most common)
Prediabetes (early stage of insulin resistance)
Gestational Diabetes (during pregnancy)
Even young women with PCOS—who may appear healthy or lean—can develop insulin resistance and abnormal blood sugar levels.
The Core Link Between PCOS and Diabetes: Insulin Resistance
What Is Insulin Resistance?
Insulin is a hormone that helps glucose enter cells to be used for energy. In insulin resistance, the body’s cells do not respond properly to insulin.
As a result:
The pancreas produces more insulin
Blood insulin levels rise (hyperinsulinemia)
Blood sugar gradually increases
How Insulin Resistance Affects PCOS
High insulin levels:
Stimulate ovaries to produce more androgens
Disrupt ovulation and menstrual cycles
Increase abdominal fat storage
Worsen acne, hair growth, and weight gain
This creates a vicious cycle:
PCOS increases insulin resistance → insulin resistance worsens PCOS → diabetes risk increases.
How Are PCOS and Diabetes Related?
PCOS and diabetes are connected through multiple biological pathways:
1. Insulin Resistance in PCOS
Nearly 70% of women with PCOS have insulin resistance—even if they are not overweight.
2. Increased Risk of Type 2 Diabetes
Women with PCOS are 4–7 times more likely to develop Type 2 diabetes compared to women without PCOS.
3. Chronic Low-Grade Inflammation
PCOS is associated with persistent inflammation, which reduces insulin sensitivity and worsens glucose metabolism.
4. Hormonal Imbalance
Elevated insulin increases ovarian androgen production, which further disrupts metabolism and reproductive health.
How Does Sugar and Glucose Affect PCOS?
High sugar intake plays a major role in worsening PCOS symptoms.
Effects of Excess Sugar on PCOS
Triggers insulin spikes
Worsens hormonal imbalance
Increases androgen production
Promotes fat storage
Causes irregular periods
Increases acne and unwanted hair growth
Hidden Sources of Sugar to Watch Out For
Refined carbohydrates (white bread, pasta, bakery items)
Packaged and processed snacks
Sugary beverages and fruit juices
Desserts, sweets, and chocolates
Managing blood sugar levels is one of the most powerful natural strategies to manage PCOS and prevent diabetes.
Can Stress Cause PCOS?
Stress does not directly cause PCOS, but it can trigger and worsen symptoms significantly.
Stress–Hormone Connection
Chronic stress raises cortisol levels, which:
Increases insulin resistance
Disrupts ovulation
Promotes weight gain
Affects thyroid and adrenal health
Stress also leads to emotional eating, sugar cravings, and poor sleep—further increasing diabetes risk in PCOS.
Stress Management for PCOS
Mindfulness and meditation
Adequate sleep (7–8 hours)
Gentle exercise like yoga
Breathwork and relaxation practices
Adaptogenic herbs
Ayurvedic Perspective on PCOS and Diabetes
Ayurveda views PCOS as an imbalance of Kapha and Vata dosha, along with impaired Agni (digestive fire) and toxin accumulation (Ama).
Ayurvedic Goals for PCOS Management
Improve insulin sensitivity
Balance hormones naturally
Detoxify the reproductive system
Reduce inflammation
Manage stress and improve digestion
Recommended Ayurvedic Support: Nari Urja
For women looking for a natural, holistic solution for PCOS and hormonal imbalance, Nari Urja is a specially formulated Ayurvedic supplement designed for women’s health.
Key Benefits of Nari Urja
Supports hormonal balance
Helps regulate menstrual cycles
Improves insulin sensitivity
Supports ovarian and uterine health
Reduces stress-related hormonal fluctuations
When combined with a balanced diet, exercise, and stress management, Nari Urja can be an effective long-term support for PCOS care.
Lifestyle Tips to Prevent Diabetes in PCOS
1. Diet
Choose low-glycemic foods
Increase fiber and protein intake
Avoid refined sugar and processed foods
Eat regular, balanced meals
2. Exercise
Strength training and brisk walking
Yoga and stretching for hormonal balance
Consistency over intensity
Read More – PCOS and PCOD Exercises at Home
3. Sleep
Aim for 7–8 hours of quality sleep
Maintain a regular sleep schedule
4. Supplements & Herbs
Ayurvedic formulations like Nari Urja
Always under medical or Ayurvedic guidance
Final Thoughts
PCOS and diabetes are closely linked—but the good news is that both are manageable and reversible with the right approach. Early awareness, lifestyle changes, stress management, and natural Ayurvedic support can make a powerful difference.
If you’re looking for a gentle yet effective way to support hormonal balance and metabolic health, Unicare’s Nari Urja can be a valuable addition to your PCOS wellness journey.
Your hormones don’t define your limits—the right care defines your healing.
Related Products
Nari Urja pack of 3: Ayurvedic Syrup for Hormonal Imbalance & Irregular Period
Frequesntly Asked Questions
PCOS and diabetes are connected through insulin resistance. High insulin levels worsen hormonal imbalance in PCOS and increase the risk of Type 2 diabetes.
Excess sugar causes insulin spikes, increases androgen levels, disrupts ovulation, and worsens PCOS symptoms like weight gain, acne, and irregular periods.
Stress does not directly cause PCOS, but chronic stress worsens hormonal imbalance, increases insulin resistance, and aggravates PCOS symptoms.
Yes, women with PCOS have a higher risk of developing prediabetes or Type 2 diabetes at an early age due to long-term insulin resistance.